What Covid19 patients can do to keep Mucormycosis away ?
Covid19 patients who have recovered or still active Covid19 patients are going through Mucormycosis, a deadly infection, caused due to excessive use of steroids in treating diabetic patients treated for Covid19. Doctors specialising in ENT, dentistry and neurologists are seeing this spike in the past few months.
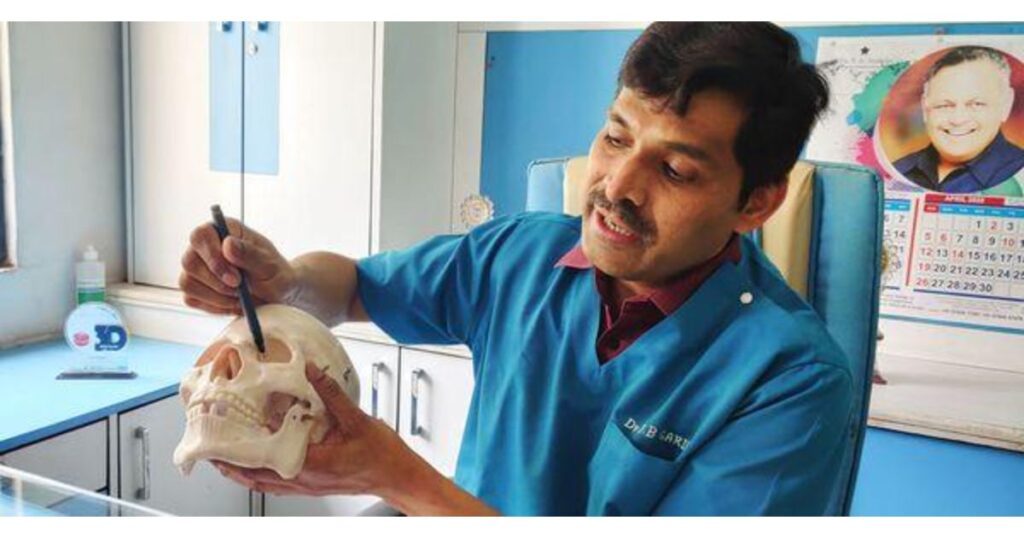
Pune Pulse spoke to some oral maxillofacial surgeons from Pune and Pimpri who are treating such patients and have observed the spike.
Dr Yashwant Ingale, head, dental department, Yashwantrao Chavan Memorial Hospital, Pimpri said, ‘Mucormycosis is a type fungal infection caused by the fungi in the order Mucorales. Air borne spores land on nasal/oral mucosa if immunologically incompetent spores are not contained by phagocytic response and gemination ensues. Exact cause of post covid mucor mycosis is unknown but may be because of immunosuppression caused by Covid, high dose of steroids, drug induced – Remdesivir , tocilizumab or even because of increase in serum iron load seen because of inflammation due to cytokine storm in covid cases. Mucormycosis is deadly and has mortality up to 50%With out surgery the mortality is 100%.’
Dr J B Garde, head, maxillofacial department, M A Rangoonwala Dental College, Azam Campus, Camp Pune said, ‘Cases of Mucormycosis are on rise in Pune, which is a deadly fungal infection putting the life of several patients in risk. It is suggested that before giving covid19 patients discharge, X ray of their mouth and PNS (Para Nasal Sinus Xray) must be done to avoid complications in such patients. Dr Dattaprasad Dadhe, another oral maxillofacial surgeon from M A Rangoonwala college too suggested that early diagnosis can save patients from further pain.
Dr Kiran Gadre and his son Pushkar Gadre, both maxillofacial surgeons operating from Tilak Road Pune have been conducting at least 4-6 surgeries everyday mainly treating Mucormycosis patients.
Dr Pushkar said, ‘It is painful to see patients as young as 30 years to get treated for this deadly infection. It is a new and not so known infection, and with only a few medicines working on it, becomes more difficult to treat. The surgeries are lengthy and also might prove fatal in some cases. Hence, it is highly recommended that Covid 19 patients should visit their dentists for any slightest chance of any symptoms in case of Mucormycosis. timely diagnosis and treatment can definitely help the doctors in reducing the infection.’
Dr Garde further stated that in various hospitals in Pune, dental clinics, more than 1000 patients have been found suffering from Mucormycosis. Since, it is not known by many, patients are losing eyesight, teeth, jaw, eyes and loss of lives too has happened in severe cases.

Government should create SOP :
The government must create an SOP regarding this infection and should make us all aware about the treatment as well as the line of treatment. To save a patient from Mucormycosis, doctors from various sections such as physician, Covid specialist, dental clinic, oral maxillofacial, ENT specialist, neurosurgeon need to work together.
What happens when Mucormycosis affects a body ?
It mostly affects maxilla but some mandibular cases are also being reported.
Signs and symptoms –
Mobility in teeth with or without periodontal abscessOpG may be completely normal Nasal discharge Palatal or nasal mucosa necrosis or black eschar Perforation in palatal mucosa Sinusitis Low grade fever Uncontrolled diabetes, cancer, HIV, Hepatitis, and patients on steroids, cyclosporine and such medicines which makes our immunity low, are the factors responsible for such fungal growth.
How does this affect ?
Spread of Mucormycosis is rapid and can affect maxillary alveolus, maxillary sinus, orbit and eventually intracranial involvement can take place
As it spreads upwards it can cause chemosis, proptosis, blindess, cavernous sinus thrombosis , cerebral ischemia, infarction and death.
As tooth aches or extraction can be associated with onset of symptoms dentist should be extremely vigilant in diagnosing such cases Thus history undertaking and prompt consultation plays a vital role in early diagnosis.
How to diagnose it ?
The best way to diagnose it is through :Fungal culture and biopsy/Endoscopic biopsy from sinus MRI is favourable than CT scan to diagnose soft tissues and vascular structures
How to manage the treatment ?
Management involves Surgical part : – Surgical debridement of the affected area – Hemi / Total maxillectomy – Debridement of maxillary sinus – Orbital Excentration – Endoscopic debridement of Ethmoid, Sphenoid sinus
Medical management Early Administration of antifungal agent -Amphotericin B with strict monitoring of serum creatinine and urea as it highly nephrotoxic
Newer agents s/a liposomal or liyophillised amphotericinB preferred as it less nephrotoxic
Surgery also leads to facial deformity and subsequent rehabilitation procedures are needed
It will affect patients financially and emotionally to great extent.
What Covid19 patients can do to keep Mucormycosis away ?
All post patients in post Covid care should get a regular dental check up done and Wearing clean mask is a must Oral hygiene must be maintained by brushing thrice daily and using mouth wash at regular basis.









